So your brain injury case involves diffusion tensor imaging…now what?
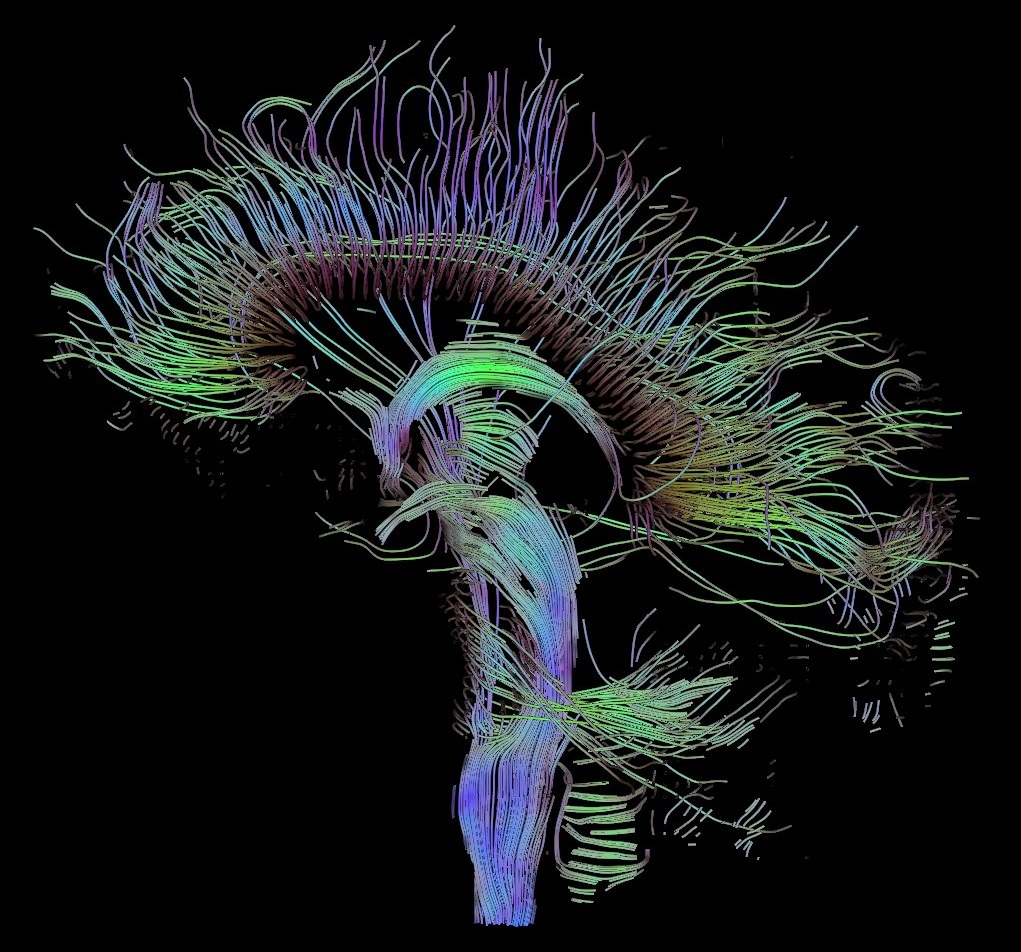
Defense attorneys and claims professionals evaluating traumatic brain injury claims are likely to come across a form of advanced neuroimaging known as diffusion tensor imaging (DTI). Diffusion tensor imaging uses data from MRI sequences to measure and patterns of water diffusion throughout brain tissue. It uses that data to map the structure of white matter tracts in the brain and draw broader conclusions about the integrity of—or subtle injuries to—those white matter tracts. The resulting colorful three-dimensional images may make for striking demonstrative evidence, but these often bely the complexity of this neuroimaging modality and what it means for the ultimate questions in a personal injury case—as well as the admissibility of DTI studies and expert opinions derived from them under Daubert v. Merrell Dow Pharmaceuticals.
In a recent column in Nautilus, “An Existential Crisis in Neuroscience,” writer Grigori Guitchounts discusses how technological advances in neuroscience are outpacing our ability to make sense of the incredible volumes of data researchers are now able to uncover about the brain’s structure and function. As he notes, “Technology has made it easy for us to gather behemoth datasets, but I’m not sure understanding the brain has kept pace with the size of the datasets.”
The column describes further conversations with researchers involved in the field of connectomics, or attempts to map out brain structures at the level of neurons to create a “wiring diagram.” Those researchers note the lack of clear understanding of how brain structure relates to psychiatric illnesses like schizophrenia, and their attempts to use machine intelligence to understand the relationship between structure and function. Despite decades of progress and access to more detailed data than ever about how the brain is composed, a holistic understanding and ability to apply that data remains elusive. As Guitchounts notes, “The machines we have built—the ones architected after cortical anatomy—fall short of capturing the nature of the human brain. But they have no trouble finding patterns in large datasets.”
Proponents of diffusion tensor imaging’s forensic use in litigating traumatic brain injury claims often tout its sensitivity, or ability to identify subtle changes in brain structures, at a degree that was previously unattainable by other structural imaging methods such as computed tomography (CT) or “standard” MRI sequences like T1, T2, SWI, and FLAIR. But, proponents miss the fact that once a lesion—often described as an area of reduced fractional anisotropy, in neuroradiology parlance—is identified on DTI, its significance in the particular case is not always entirely clear. There is not always a definitive correlation between an identified white matter lesion and neurocognitive complaints, whether identified by neuropsychological testing or not. This is especially true given that white matter lesions have a host of other causes unrelated to trauma—such as hypertension, pre-existing psychiatric conditions, or even the normal aging process. And, in our firm’s work in litigating traumatic brain injury claims nationally, we have occasionally seen DTI studies that describe a totally normal brain despite the fact that other imaging modalities like MRI have documented obvious structural brain damage in a particular individual. In such cases, the inability of DTI’s high-resolution data to identify lesions where they clearly should exist raises questions about the clinical and forensic significance of single, isolated lesions in concussion cases.
In evaluating the strength and admissibility of expert opinions interpreting diffusion tensor imaging, one should be aware of the host of potential issues surrounding DTI and its interpretation in any particular case, including partial volume effects, the multiple comparisons problem, normative datasets, and mapping errors. And, in addressing whether DTI evidence satisfies Daubert and Fed. R. Civ. P. 702 in a case, attorneys should consider whether a DTI study merely “finds a pattern in a large dataset” without a clear understanding, based on actual science, of how that pattern correlates with an identified neuropsychological deficit or symptom that is at issue in the case. DTI abnormalities are not per se evidence of a TBI, and an expert who opines that they are likely expresses a degree of certainty that goes beyond the current scope of neuroscientists’ understanding about the relationship between brain structure and function.